Researchers and clinicians from the Walter and Eliza Hall Institute and The Royal Melbourne Hospital provide the first evidence in humans that a nasal spray vaccine could prevent type 1 diabetes.
World first discovery
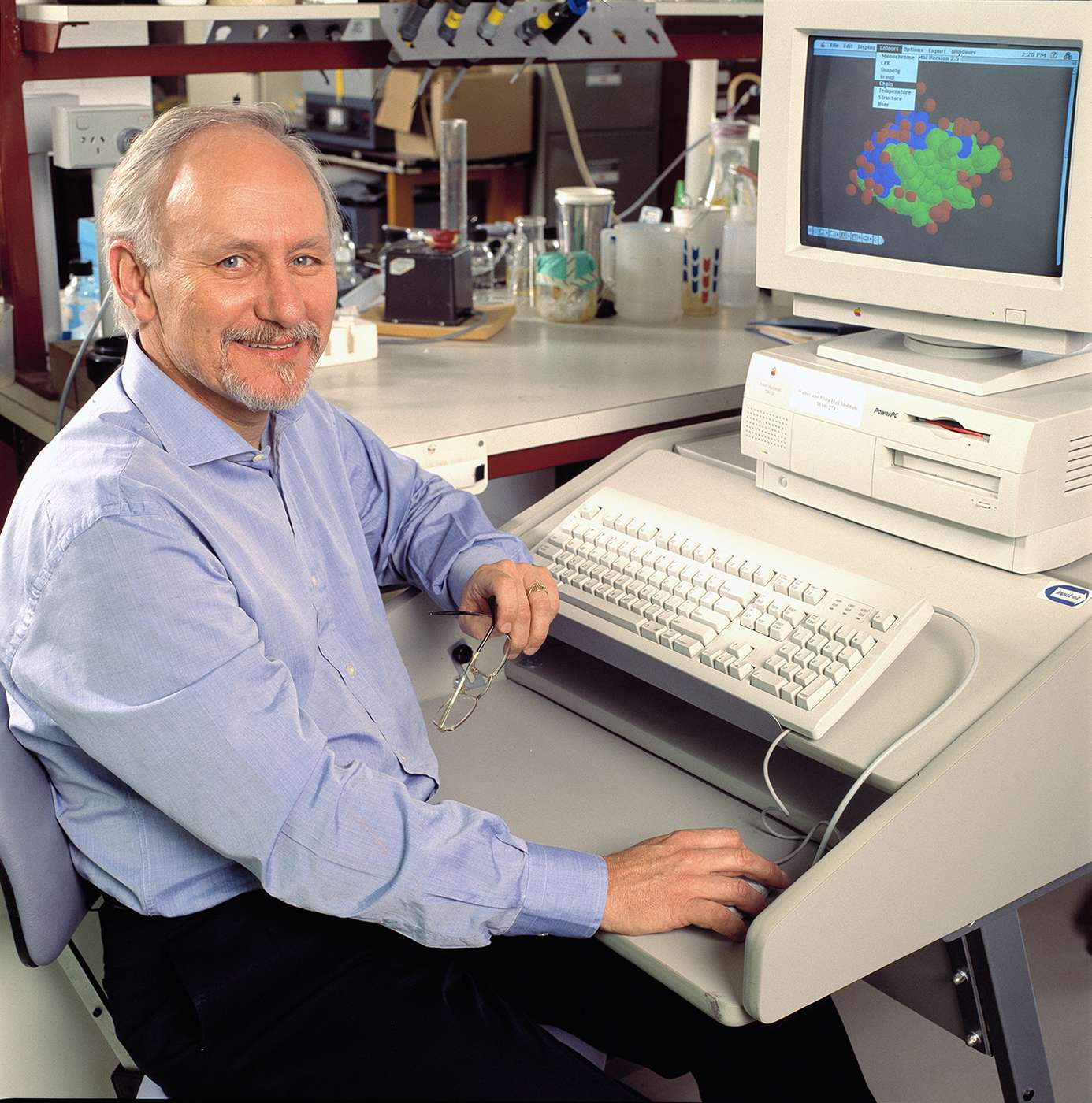
The team, led by Professor Len Harrison with Professor Peter Colman and Dr Spiros Fourlanos, demonstrate that the nasal insulin vaccine suppresses the immune response to insulin in people who have early type 1 diabetes.
“It’s the first time that anyone has really shown that this novel type of vaccine approach can actually change the immune response to something that in their body is causing autoimmune disease,” Harrison says.
Diabetes dilemma
Type 1 diabetes occurs when the body’s immune system attacks and kills the beta cells in the pancreas that produce insulin. Crucially, insulin itself is a specific target of the immune attack that kills beta cells.
Insulin is a vital hormone that moves glucose from the bloodstream into the body’s cells, giving them the energy needed for daily life. Lack of insulin leads to serious health problems and people with type 1 diabetes require daily insulin injections to survive.
The nasal insulin vaccine sensitises people at risk of developing type 1 diabetes to make a protective immune response to insulin.
“If the nasal insulin vaccine proved to be effective it could prevent many people from developing type 1 diabetes,” Harrison says.
“Our approach has been to try to switch off the body’s inappropriate immune response to insulin, which we think is the underlying cause of type 1 diabetes in children,” he says.
“The big advantage that we have in type 1 diabetes is that we can now identify children at an early stage, years before they turn up with symptoms, giving us a window of time in which we can try to prevent it developing.”
Hijacking the system
The vaccine is administered through the nose, where it interacts with the nasal lining, part of the body’s mucosal barrier.
Here it switches on a protective immune response that dampens inappropriate, tissue-destructive immune responses.
“The mucosal ‘barrier’ is the size of a tennis court, and is the primary site of our interactions with the environment,” Harrison says.
“One of the key jobs of this barrier is to sort the wheat from the chaff – alerting the immune system to real danger, yet teaching it to tolerate things that are best ignored.”
Harrison says the nasal vaccine hijacks this system.
“The nasal vaccine is designed to take advantage of the mucosal barrier’s role in teaching tolerance. It switches on what we call regulatory T cells, which have a vital role in dampening the immune response when it is activated inappropriately.”
Restoring tolerance
In the study, Harrison and his colleagues tested 52 adults with early type 1 diabetes over one year, giving half the nasal insulin vaccine and half a placebo. Although the participants were initially not at the stage of requiring insulin injections they had evidence of immunity to the insulin-producing beta cells in the pancreas.
They found those who’d been given the vaccine had a suppressed immune response to insulin when it was eventually injected for the treatment of high blood glucose.
“The results showed that the vaccine restored immune tolerance to insulin,” says Harrison. “When subsequently given insulin by injection, the participants who had received the nasal insulin vaccine were desensitised to insulin.
“The study provides proof-of-principle for the type 1 diabetes prevention trial (intranasal insulin trial II or INIT II) currently being conducted in Australia, New Zealand and Germany.”
“We’re very excited because these latest results encourage us that we are on the right track to finding a vaccine for type 1 diabetes.”
Preventing diabetes
The INIT II study began in 2006 and in 2014 finished recruiting participants. The results probably won’t be known for several years because the trial is intended to test whether the vaccine prevents diabetes developing.
“We have enrolled 110 children who are at a high risk of developing diabetes because they have already developed autoantibodies to insulin or other antigens implicated in type 1 diabetes,” Harrison says.
“The trial will determine whether the nasal insulin vaccine delays or prevents the onset of type 1 diabetes.”
“It has been a long journey, but each step – to identify children at risk, to show that insulin is a key autoimmune target, and to show that nasal insulin is indeed a ‘negative vaccine’ that induces immune tolerance to insulin, has been successful and moved us forward to what we hope will be the ultimate goal – the prevention of type 1 diabetes.
The INIT II study is sponsored by Melbourne Health and is funded by the National Health and Medical Research Council and the Juvenile Diabetes Research Foundation.
Determining the cause of diabetes
In 2015 Australia’s largest study into the causes of type 1 diabetes – ENDIA – began with Harrison as a chief investigator. ENDIA will follow babies before and after they are born to understand how environmental factors interact with genes to increase the baby’s chance of developing type 1 diabetes.
“Type 1 diabetes in children is twice as common as it was 20 years ago,” Harrison says.
“Our environment has changed and this has made it more likely for a child at risk to develop type 1 diabetes.
If we can understand what factors in the environment are harmful or protective, and how they interact with our genes, we can modify the environment or develop new tools to prevent type 1 diabetes.”