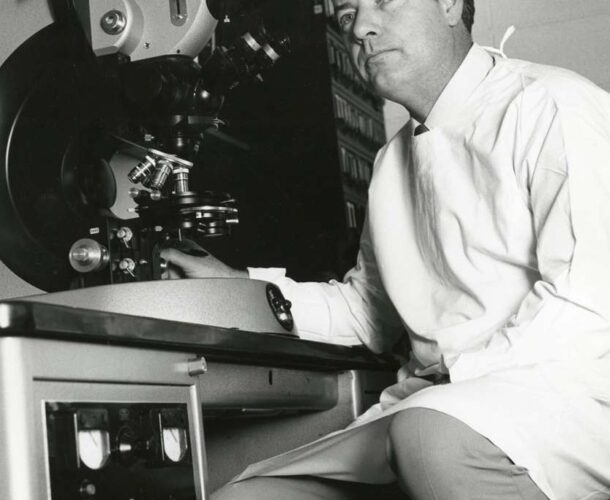
From his early years at the Walter and Eliza Hall Institute, Professor Don Metcalf focused on conquering cancer.
Supported by the Carden Fellowship from the (then) Anti-Cancer Council of Victoria, the terms of his appointment in 1954 were to “find the cause and cure of cancer”.
While much of the institute was immersed in the “golden age of immunology”, Metcalf was committed to his cancer studies, and began investigating the role of the thymus in leukaemia development.
Looking back at this early work, he already exhibited the defining characteristics of meticulous experimental design and execution, and his aptitude as a researcher was obvious.
Mr Thymus
The thymus was something that generated little interest at the time. It was considered a ‘vestigial’ organ with no useful function, a ‘graveyard’ for dying and dead lymphocytes.
Metcalf, or ‘Mr Thymus’ as he was known then, spent the first 10 years of his career studying the thymus and the immune cells now known to populate it.
It wasn’t until 1960-61 that future institute researcher Professor Jacques Miller, then a PhD student at the Institute for Cancer Research, UK, discovered the thymus was crucial for the development of normal immune function early in life.
Metcalf’s work focused more on the thymus and its role in leukaemia, for which his studies were (and are) considered definitive. Yet they also provided fundamental information on the functions of the normal thymus.
Among the more interesting findings of his work was that thymus tissue transplanted into a new host becomes populated by lymphocytes from that new host. This suggests a ‘stem cell’ from the bone marrow of the new host was the likely source, and would be later proven by Miller and Professor Graham Mitchell.
A cellular graveyard
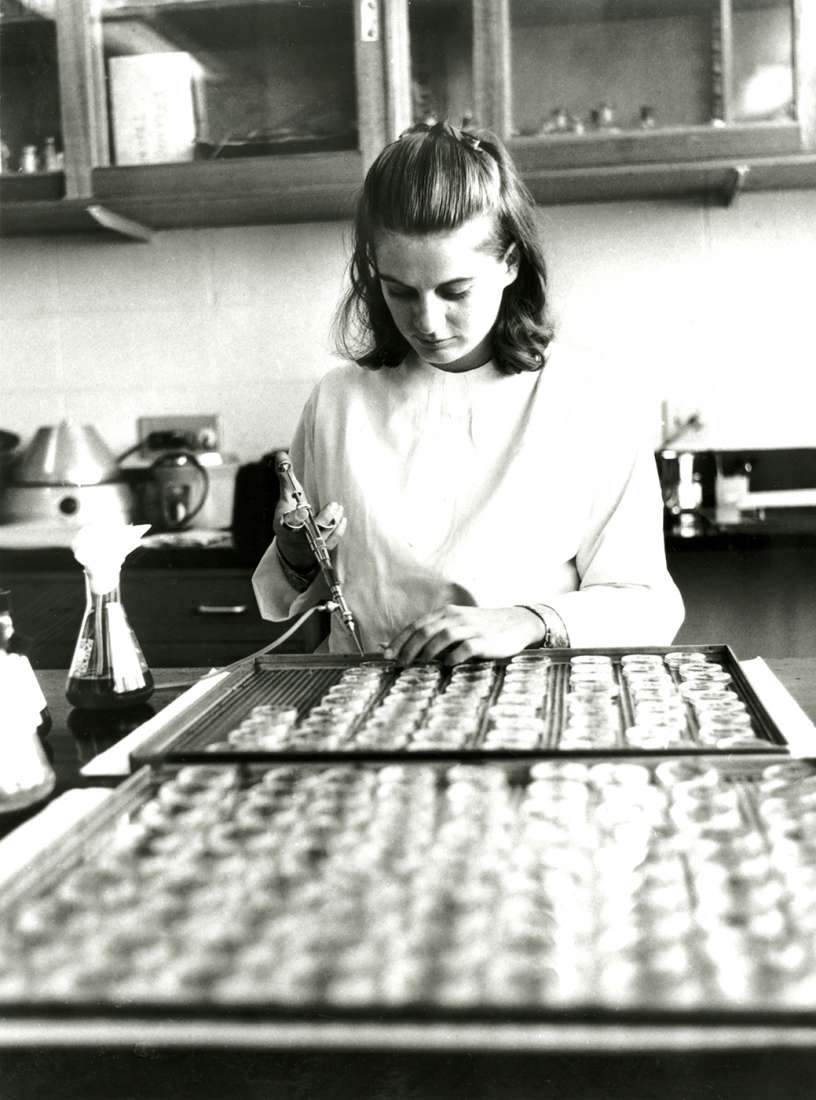
In 1966, Metcalf and his associate Margaret Brumby (then Wiadrowski) report in a study published in Cancer Research. Their meticulous research shows the thymus regenerates about one third of its cell numbers each day but that 99 per cent of those developing cells die soon after.
So there was a paradox. Though the thymus appeared to be the factory and homing ground of lymphocytes (later found to be T cells), vast numbers of lymphocytes also met their death there shortly after they were born.
Few at the time accepted that a biological system could be that wasteful and it was many years before this culling of T cells was accepted as the necessary price of immunity.
As Don later recollected:
“Well, if you believe the immunologists they will tell you the following story.
The thymus makes one sort of white cell called the T lymphocyte, T for thymus. And T lymphocytes protect you against viruses and foreign tissue grafts and possibly against some sorts of cancer. Now, most of the cells that get made in the thymus die there, within a couple of days. Why do they die? Because they are attacking their own tissues and so they have to be assassinated … The few that are not, the few that are really interested in looking at strange things like viruses, get out into the body but once they’re out there they become long lived memory cells and they live for the lifespan of the person.”
This description highlights the highly inefficient process that the body uses to select our immune repertoire, which is now a cornerstone of immune theory.
Soon after this work is published, Metcalf and his collaborator from The University of Melbourne Ray Bradley make the discovery that will completely change the focus of Metcalf’s work. He will move on from the thymus, and focus on white blood cells, the factors that help them grow, which will lead to a revolution that has helped more than 20 million people worldwide.