Professor Paul Waring attributes his success in medical research to three things: the pathology training that’s provided him with a detailed understanding of human disease; his clinical experience, which helps him ask important questions; and his experience in the pharmaceutical industry that taught him to focus on improving health outcomes.
But none of it would have happened had he not won a scholarship to leave his native UK to study geology at the University of Western Australia and met a girl who was studying medicine.
“I was fascinated by the natural sciences but she inspired me to become a doctor,” Waring recalls. “So after getting great grades in first year, I switched to medicine. As a fourth year student, I became interested in pathology, later choosing it as my specialty.”
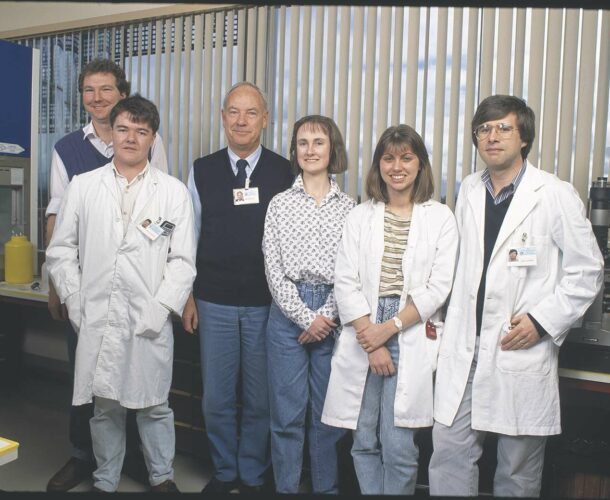
On the pathway to the Walter and Eliza Hall Institute laboratories
During the next five years he reported 12,000 surgical pathology cases, conducted 400 autopsies and “learned to diagnose almost any human disease just by looking down the microscope.” In 1989 a mentor, seeing Waring’s zeal for inquiry, suggested he undertake a PhD at the Walter and Eliza Hall Institute with the now late Professor Donald Metcalf, whose lab had recently discovered a new molecule, leukaemia inhibitory factor (LIF).
Between Waring accepting the offer and arriving in the lab, Metcalf had also discovered LIF was a powerful stimulator of platelets, which are responsible for blood clotting. Waring then set out to study the effect of LIF on platelets.
“I spent about nine months doing a lot of experiments I made a mess of,” Waring recalls.
Meanwhile, biochemist Professor Nick Nicola’s lab had developed an assay, or test, for detecting LIF. With ethics approval, Waring then screened “over 1000 random blood samples” obtained from the local pathology labs for LIF. “And then, bingo! One day there was a positive sample.” This came from a child with meningococcal septicaemia — a bloodstream infection caused by the meningococcal bacteria.
“That was the first clue that LIF was involved in the body’s innate immune response.”
Waring found LIF in the blood of more septic patients; the more severe the disease, the greater the amount. He also tested samples of joint fluid from patients with rheumatoid arthritis and amniotic fluid from pregnant women with intrauterine infections and found that LIF was often associated with inflammation.
He tested LIF in mice injected with lethal doses of live bacteria. He found LIF had no effect when given at the same time or after the lethal injection but, unexpectedly, LIF prevented death in all mice if given at least four hours beforehand. He again figured LIF played a role in regulating the immune system, presumably to prevent an overzealous inflammatory response to infection. “No-one took any notice though,” Waring grins.
On the move
After pursuing a postdoctoral fellowship in molecular pathology at Stanford University he later returned to the University of Melbourne and in 2001 became the Director of Pathology at the Peter MacCallum Cancer Centre. In 2004, he was headhunted by San Francisco-based Genentech, the world’s first and most successful biotech company, which recruited him to run their pathology department and set up their diagnostics division.
“Working at Genentech was like doing three PhD’s simultaneously.” Waring became “an expert in personalised medicine,” spearheading the company’s efforts to harness the new genetic technologies and other biological tools to identify which patients benefited from their drugs.
Advances in breast and ovarian cancer research
In 2005, scientists from KuDOS Pharmaceuticals published breakthrough findings that a new drug could arrest the growth of cells bearing mutant BRCA1 or BRCA2 genes, which are associated with breast and ovarian cancer. Waring was part of Genentech’s due diligence team that flew to Cambridge to investigate the new drug with a view to licensing it or buying the company.
“We underestimated its importance and value and another company outbid us. I always felt we missed a great opportunity because the drug should work in non-BRCA carriers with similar tumours.” Up to half of all patients with the most common and lethal form of ovarian cancer have these “BRCA-like” tumours.
Returning to collaborate with the Walter and Eliza Hall Institute
Now Waring is Chair of Pathology at the University of Melbourne and collaborating with the Walter and Eliza Hall Institute’s Associate Professor Clare Scott. They have developed an assay to identify patients with “BRCA-like” tumours and have convinced AstraZeneca to provide the drug for a clinical trial to see if it works on this subgroup.
Waring began his work initially unaware that Scott was pursuing the same research goals. Later, they joined forces, each bringing different skills to attack the problem. “Some people feel threatened when they learn you’re working in the same space, but Clare was very receptive and encouraging. I think that’s the mark of a good scientist.”