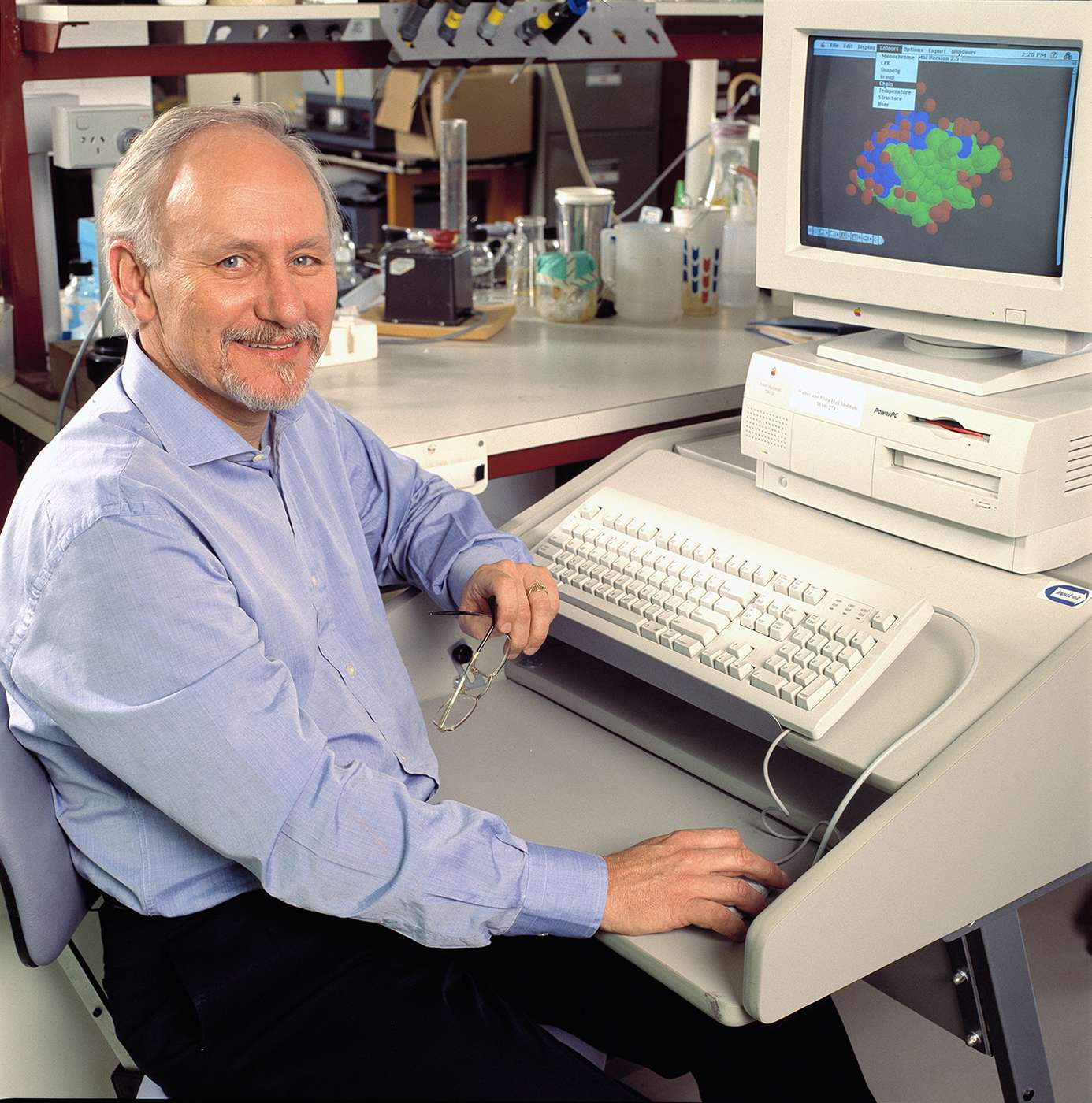
At his cherry farm in Victoria’s Yarra Valley, internationally lauded diabetes researcher Professor Len Harrison makes bronze sculptures. While his early pieces were figurative, lately the clinician-scientist from the Walter and Eliza Hall Institute prefers abstract forms inspired by nature. A sculpture might resemble a leaf or flame, Harrison explains, “but look closely and you see a human form, say the arm of a woman cradling a baby”.
His evolution as an artist bears some resemblance to his evolution as a scientist, chipping away from various medical vantage points at type 1 diabetes, an autoimmune disease in which the pancreas does not produce sufficient insulin, a hormone needed to break down sugar (glucose) for the body’s cells. Harrison has come at type 1 diabetes – which he sees as a “portal to understanding other autoimmune diseases”—from endocrinology and immunology, and is now probing the interaction between DNA and the environment by tracking at-risk babies in the womb.
His goal is a vaccine to prevent type 1 diabetes. “The disease typically develops in children and teenagers and requires daily insulin injections for survival. It also causes significant long-term complications involving the eyes, kidneys and blood vessel damage, at great cost to the individual and the community.”
Attacking type 1 diabetes
Harrison began attacking diabetes at The University of Melbourne in the 1970s as a budding endocrinologist, a discipline that struck him as “more mechanistic and less empirical” than others. “I now realise I was among the first to describe the insulin receptor on human cells,” says Harrison of his early research, “to identify the special molecules on cells called receptors that interact with insulin and transmit its signal into the cell.”
His work led to a prestigious CJ Martin Fellowship to undertake postdoctoral research at the National Institutes of Health (NIH) in Bethesda, Maryland. There he and his colleagues found that in rare forms of diabetes the immune system makes antibodies to the insulin receptor, which block the receptor and stop the insulin from working. Harrison used these antibodies as a lab tool to separate the insulin receptor from the thousands of other molecules in the cell and study its structure.
His professional life might have taken a different turn had he stayed at the NIH. He had begun collaborating with J. Craig Venter, the blockbuster scientist known as the first to map the human genome in 2001.
“This was the early 1980s,” Harrison explains, “and my friend J. Craig Venter was interested in the new science of DNA technology. And he said, ‘Why don’t we get into this?’” But Harrison “had five kids and no money” and just been offered a relatively well-paid position as an endocrinologist at The Royal Melbourne Hospital.
A vaccine for diabetes
In 1987 Sir Gustav Nossal recruited him to head the Walter and Eliza Hall Institute’s restyled Burnet Clinical Research Unit where, for the first time in Australia, he developed tests to detect children at risk of developing type 1 diabetes. “We followed those children all the way to diabetes, and learnt a lot about the disease before it appeared,” Harrison explains.
“Then towards the end of the 1980s, we started to look at ways to prevent diabetes in young people who were at high risk but otherwise well.”
Meanwhile, “a circumstantial case was building that T cells” — white blood cells that scan for abnormalities and infections – “were ‘the real killers’ of insulin-producing beta cells in the pancreas. And that insulin itself was a target of these killer T cells”.
So here we have the immune system attacking insulin. And our idea was somehow to turn insulin from a target into a therapeutic tool, to get the immune system to see insulin in a protective way, to build tolerance to it.
Indeed, when Harrison and colleagues genetically engineered diabetes-prone mice to expose the developing immune system to insulin, the immune system eliminated the T cells that attack insulin and the mice were protected from diabetes. This showed that insulin, paradoxically, could prevent type 1 diabetes – but the genetic approach was not ethical in humans and another way had to be found.
It involved a nasal insulin vaccine, which Harrison had shown protected type 1 diabetes-prone mice. It works because the mucous membranes in our bodies contain a “special immune system that prevents us from reacting badly to what we breathe in or eat.”
“So we give insulin nasally. Now the bad guys are T cells that react to insulin and cause inflammation that kills off the beta cells. The good guys are T cells called regulatory T cells, stimulated by nasal insulin, that dampen inflammation.”
An international trial of the nasal vaccine to see if it will prevent type 1 diabetes commenced in 2006 and is nearing completion. Earlier, Harrison and colleagues had shown the nasal vaccine approach was safe and indeed stimulated protective immunity to insulin in humans.
Trial set to identify cause of diabetes
In the past 20 years the incidence of type 1 diabetes has increased in the West, including Australia, “and that’s down to the environment because our genes themselves haven’t changed.” Harrison cites the example of Finland, a highly developed society, and its relatively undeveloped neighbour Karelia in Russia. While the residents of each place share similar genes, the incidence of type 1 diabetes in Finland is nine times higher than in Karelia.
“Chemical changes occur in the DNA in response to the environment,” Harrison explains. To identify those environmental factors, Harrison is jointly leading a nationwide study tracking 1400 babies at high risk of developing type 1 from the womb throughout early life. The ambitious study was initially supported by the National Health and Medical Research Council, and recently boosted by an $8 million grant from The Helmsley Charitable Trust, US, and local partner JDRF Australia.
The DNA and immune systems of the mothers and their offspring, and their exposure to environmental agents from infections to household detergents to diet, are being probed, so that scientists can piece together the puzzle of type 1 diabetes.