In 1983 researchers from the Walter and Eliza Hall Institute successfully purify G-CSF, one of the four CSFs molecules that stimulate white blood cells to grow.
The discovery is a major step forward in the program to isolate and purify CSFs for future treatment. It soon leads to clinical trials and, finally, approval of CSFs to treat people with cancers and immune disorders and revolutionise stem cell transplants.
Devil is in the detail
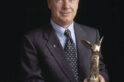
They say the devil is in the detail, and the detail led Professor Nick Nicola a merry dance for years as he persevered with trying to isolate a key protein.
The work was slow, painstaking and often frustrating, and the odds astronomical: he sought to purify a protein that was only one part in three million of the source that held it.
But success, when it came, was astronomical: 20 million cancer patients have now benefited from the new medicine that resulted from Nicola, Professor Donald Metcalf and their team on colony stimulating factors (CSFs).
Critical immune signals
CSFs are critical proteins that tell stem cells in the bone marrow to multiply and mature to boost the immune system. They are now routinely given to many cancer patients to boost their immune systems after chemotherapy (chemotherapy suppresses the immune system and leaves cancer patients vulnerable to infections).
The use of CSFs has also revolutionised transplant medicine, leading to new techniques for performing bone marrow transplants for patients with blood cancers such as leukaemia.
Making a difference
Nicola began his career in a discipline called physical protein chemistry, “a very highly specific area of research which is difficult to connect directly to human health”.
But he did want to do work that made a difference to medicine, so he accepted an offer to work on blood-cell production at the institute with Professor Tony Burgess and the man later dubbed the father of modern haemotology, the late Professor Don Metcalf.
“That seemed something that would get me much closer to direct impact on human health,” Nicola says. “This was, at the time, the leading haemotology group in the world, under Don Metcalf’s leadership.”
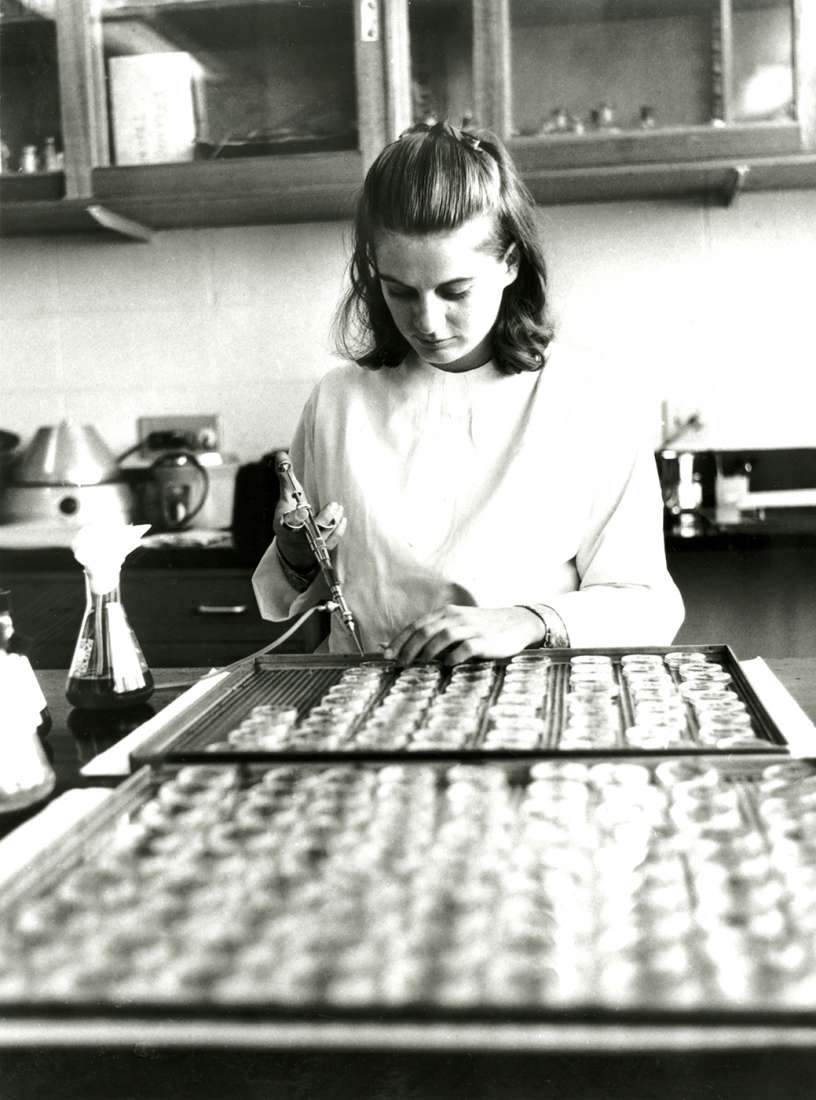
Ten years earlier, Metcalf and another colleague, Dr Ray Bradley, had discovered how to grow blood cells in petri dishes using bone marrow stem cells, the grandfather and grandmother cells that generate all the different kinds of red and white blood cells. These stem cells were then called colony-forming cells, and when Nicola joined the team, it was searching for what regulated their growth.
A Herculean task
“My first job was to sort out how many colony-stimulating factors there were,” says Nicola. “Then I focused on the colony-stimulating factor that acted on granulocytes, a particular kind of white blood cell. Purification (of granulocyte colony stimulating factor, G-CSF) turned out to be a long and difficult task. It took several years and a lot of back steps and sidesteps.
“What we didn’t appreciate at the time was the incredible amount of activity the G-CSF had. You were talking about a billionth of a gram of G-CSF that was able to do this, and you were trying to purify tiny amounts of this from massive amounts of contaminating proteins.”
The biggest problem turned out to be that the tiny amounts of G-CSF would stick to plastics and cling to test tubes. “All surfaces have a capacity to absorb a few billionths of a gram and when you got anywhere near pure, you’d lose it. Finally, we added something to it to stop it sticking, and that changed everything. We finally had a pure protein. It was just 3 millionths of a gram.”
A treatment is born
The team published the results of this work and researchers in Japan used these findings to clone the G-CSF gene, which meant it could be manufactured in large quantities.
“Now, it’s basically used to treat a whole range of cancer patients who receive chemotherapy, because chemotherapy damages white blood cells which means you have no resistance to infection. It also means you can increase the level of chemo to kill the cancer.”
Professor Metcalf later discovered that the G-CSF was taking stem cells out of the bone marrow, where they were made, and putting them into the bloodstream.
“This has revolutionised bone-marrow transplants, which can now be done with just blood transfusions rather than invasive procedures in the bone marrow,” Professor Nicola says. “You inject the G-CSF into the donor and when the stem cells enter the blood, you collect the blood and transfuse it into the patient. The process is called peripheral blood stem-cell transplantation. It’s safer and easier and, surprisingly, more effective than a traditional bone marrow transplant.”
A rare opportunity
When he looks back over his career, what Professor Nicola feels most is gratitude. “When you are in the game long enough, you realise that these things are extremely rare. You have to be very lucky, in the right place at the right time.
“There are very few people in science who can point to something that’s now a treatment for 20 million patients worldwide, which is an extraordinary change in clinical practice. I feel extremely humble and very, very lucky to have been a part of it.”